What are the parts of developing long bone?
Parts of a developing long bone are: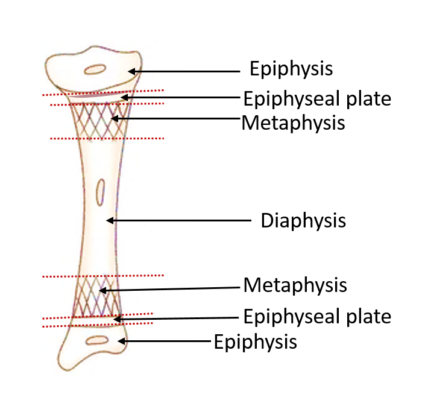
- Epiphysis:
- The ends of long bones that ossify from the secondary centre of ossification are called epiphysis.
- Epiphyses are made of spongy bone covered by a thin layer of compact bone.
2. Diaphysis:
- The elongated, cylindrical shaft of long bone that ossifies from the primary centre of ossification.
- It is made up of compact bone and encloses a tubular cavity called marrow cavity.
3. Metaphysis:
- It is the part of diaphysis that is adjacent to the epiphyseal plate.
- This is the most active site of bone formation in the developing bone.
- It has rich blood supply.
4. Epiphyseal plate:
- It is a thin plate of hyaline cartilage placed between the diaphysis and epiphysis.
- The continuous proliferation of cartilage cells in the epiphyseal plate is responsible for the growth of developing bone in length.
What is ossification and centers of ossification?
Ossification
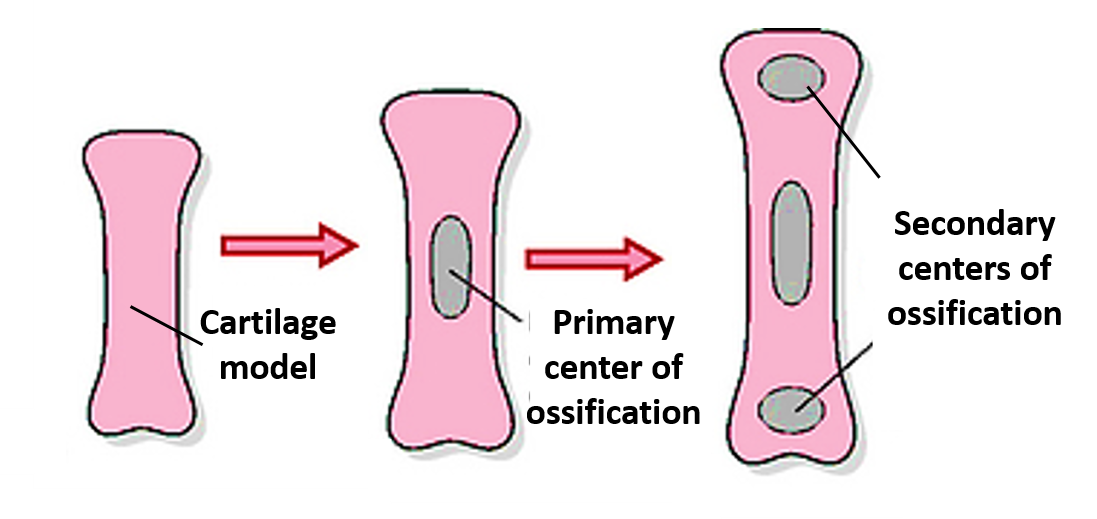
Bone ossification, or osteogenesis, is the process of bone formation. Sites where it begins are referred to as centers of ossification. There are two types of centers of ossification:
Primary center of ossification
- It is the site in the mid region of shaft of long bone where ossification begins earliest.
- It forms the main part of the bone (diaphysis in long bones).
- It usually appears before birth (usually before the end of the fourth month of intrauterine life).
Secondary center of ossification
- They usually appear after birth from which the ends of the developing long bone ossify.
- They form the epiphyses of the long bones.
- In case of femur the secondary center of ossification for the lower end appears just before birth.
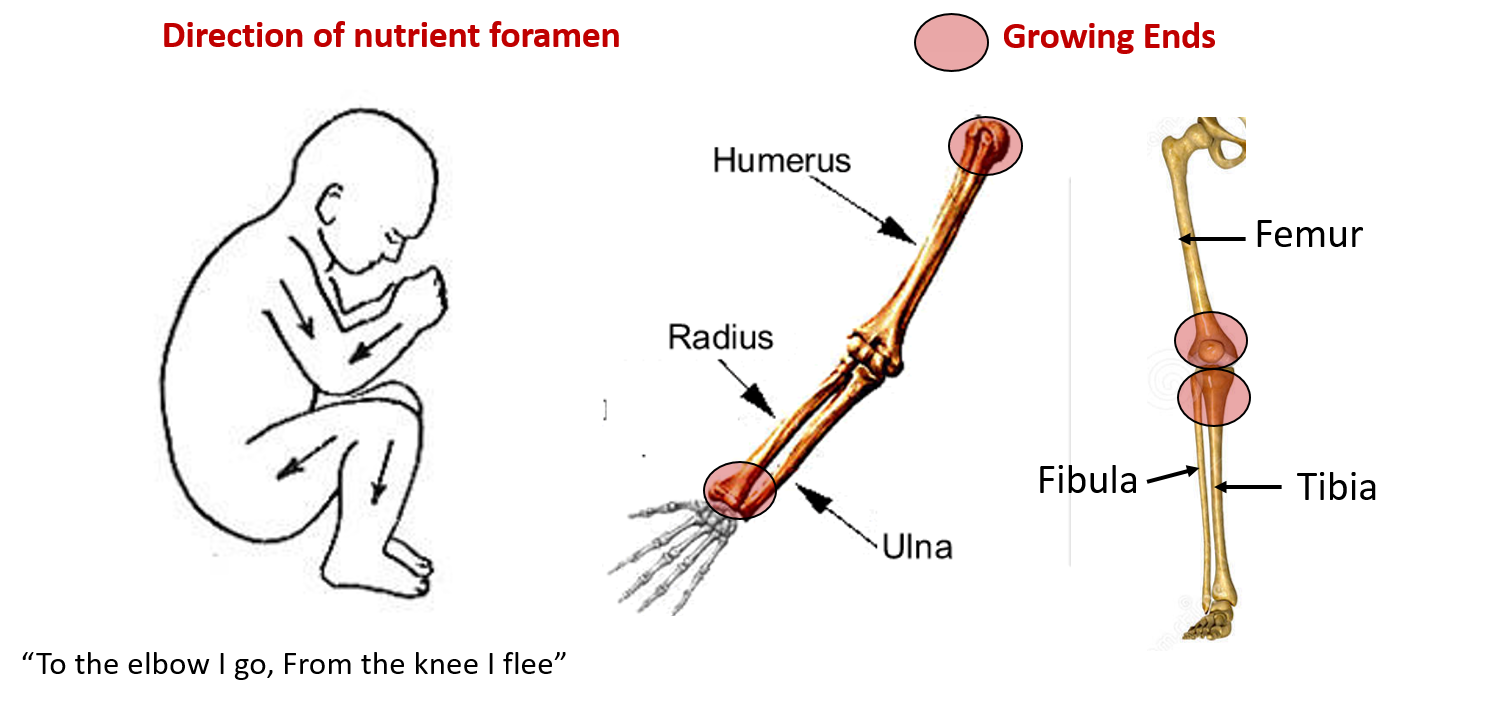
Which end of a long bone is called the growing end?
- It is that end of the long bone where the epiphysis fuses with the diaphysis later than the other end (it continues to grow in length a little longer).
- The growing end of the long bone is opposite to the direction of the nutrient foramen (exception to the rule is fibula where the nutrient foramen is directed towards the growing end).
What are the different types of ossification?
Bone formation is typically a two-step process whereby an organic matrix (osteoid/cartilage template) is initially laid down by osteoblasts and then mineral crystals are precipitated. Bone can be formed in two ways:
• Intramembranous ossification
• Intracartilagenous or endrochondral ossification
Each of these processes begins with mesenchymal tissue precursor. Intramembranous ossification directly converts the mesenchymal tissue to bone and forms the flat bones of the skull, clavicle, and most of the cranial bones. Endochondral ossification begins with mesenchymal tissue transforming into a cartilage intermediate, which is later replaced by bone and forms the remainder of the axial skeleton and the long bones.
Membranous ossification
In this type of ossification, the mesodermal model is directly converted into bone by mineralization of the matrix. Most of the flat bones such as frontal and parietal bones, parts of occipital, temporal, mandible, maxilla and clavicle bones are formed by intramembranous ossification It can be divided into the following 4 stages:
1. Mesenchymal condensation and appearance of centers of ossification: one or two centres of ossification appear in the condensed mesenchyme. The center of ossification is characterised by excessive vascularity and differentiation of mesenchymal cells into osteoblasts.
2. Formation of osteoid matrix and its calcification: osteoblasts secrete gelatinous uncalcified matrix and collagen fibers (osteoid). Calcium salts are then deposited in the osteoid. The osteoblasts trapped in mineralized matrix become osteocytes.
3. Formation of spongy (trabecular) bone: bony lamellae are formed around the blood vessels and are arranged in the form of trabeculae which are separated by spaces containing blood cells (marrow spaces). Thus spongy bone is formed.
4. Formation of compact bone and periosteum: the osteoblasts at the periphery lay down concentrically arranged bony lamellae, forming osteons (Haversian system) of compact bone (spongy bone is replaced by compact bone). Outside the compact bone mesenchymal cells form fibrous periosteum with osteoblasts on inner surface.
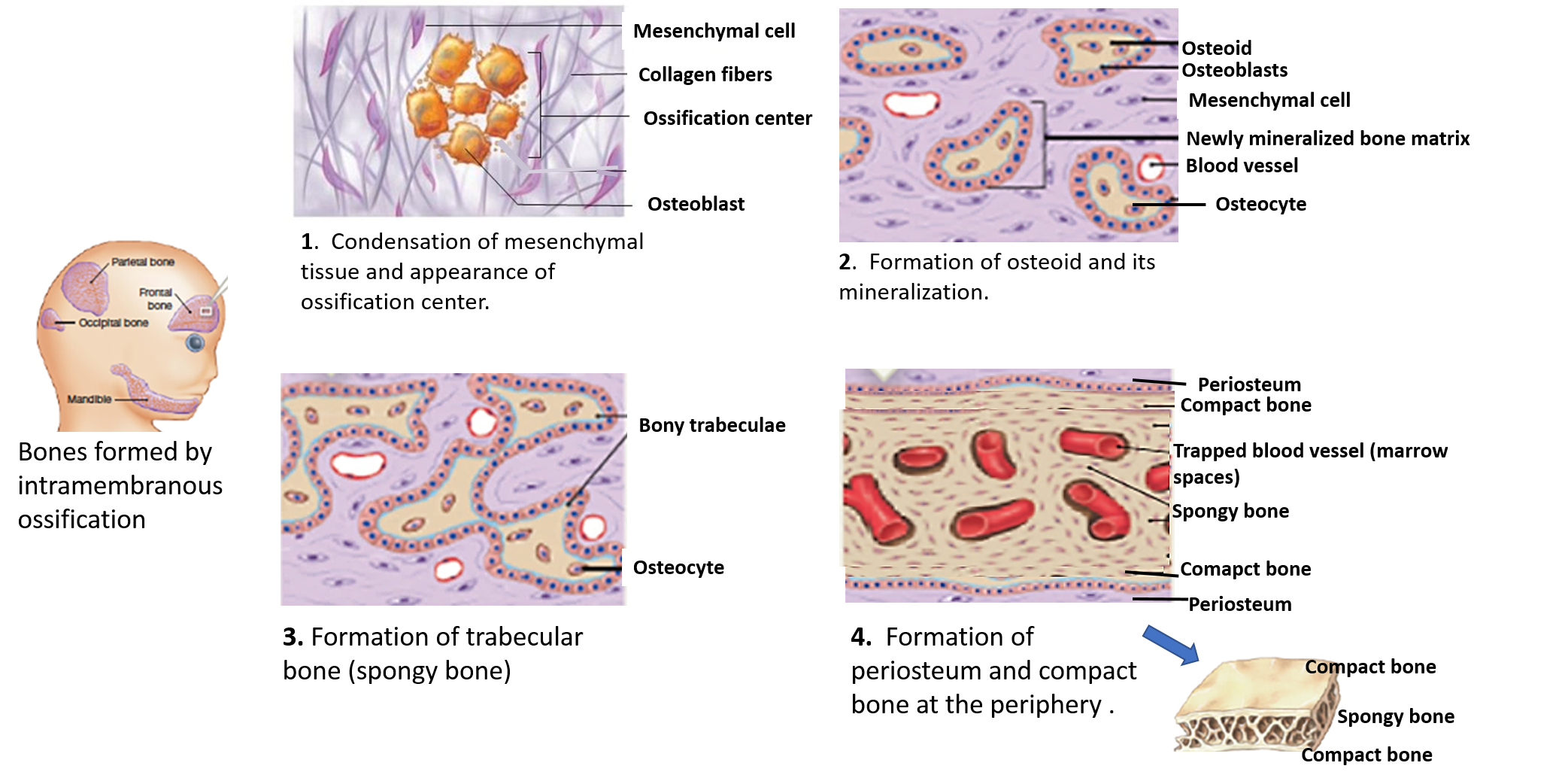
Five steps can summarize intramembranous ossification:
- Mesenchymal cells differentiate into osteoblasts and group into ossification centers.
- Osteoblasts become entrapped by the osteoid they secrete, transforming them to osteocytes.
- Trabecular bone and periosteum is formed.
- Cortical bone forms superficially to the trabecular bone.
- Blood vessels form the red marrow.
Endrochondral ossification
In this type of ossification, firstly a hyaline cartilage model of bone is formed, which is later replaced by bone. It involves the following 4 stages:
1. Chondrification: mesenchymal cells differentiate into chondroblasts, which form a hyaline cartilage model for the future bone. At the periphery mesenchymal cells for perichondrium which contains osteogenic cells on the inner surface.
2. Appearance of centres of ossification: one or more centres of ossification appear in the cartilage model. Chondrocytes near the center of the bony model begin to undergo hypertrophy and start adding collagen and more fibronectin and alkaline phosphatase, which is an enzyme that acts as a nucleator for deposition of minerals.The calcification of the extracellular matrix prevents nutrients from reaching the chondrocytes and causes them to undergo apoptosis. Chondrocytes also secrete growth factors to promote the invasion of blood vessels.
3 .Formation of Periosteal bone collar: Blood vessels carry in osteogenic cells and trigger the transformation of perichondrium to the periosteum. Osteoblasts then create a thickened region of compact bone in the diaphyseal region of the periosteum, called the periosteal collar. It is here that the primary ossification center forms.
4. Invasion of periosteal sprouts and osteogenesis: periosteal sprouts arise from deeper layer of periosteum (contain blood vessels, osteoblasts and osteoclasts) and invade the underlying calcified matrix. The osteoclast resorb the matrix to form large interconnecting spaces called marrow spaces which ultimately join together to form medullary cavity.
While bone is replacing cartilage in the diaphysis, cartilage continues to proliferate at the ends of the bone, increasing bone length. These proliferative areas become the epiphyseal plates, which provide longitudinal growth of bones after birth and into early adulthood.
5. After birth, this entire process repeats itself in the epiphyseal region, this is where the secondary ossification center forms.
The epiphyseal plate has five zones:
• Resting zone
• Zone of proliferation
• Zone of hypertrophy
• Zone of calcification and dying chondrocytes
• Zone of ossification
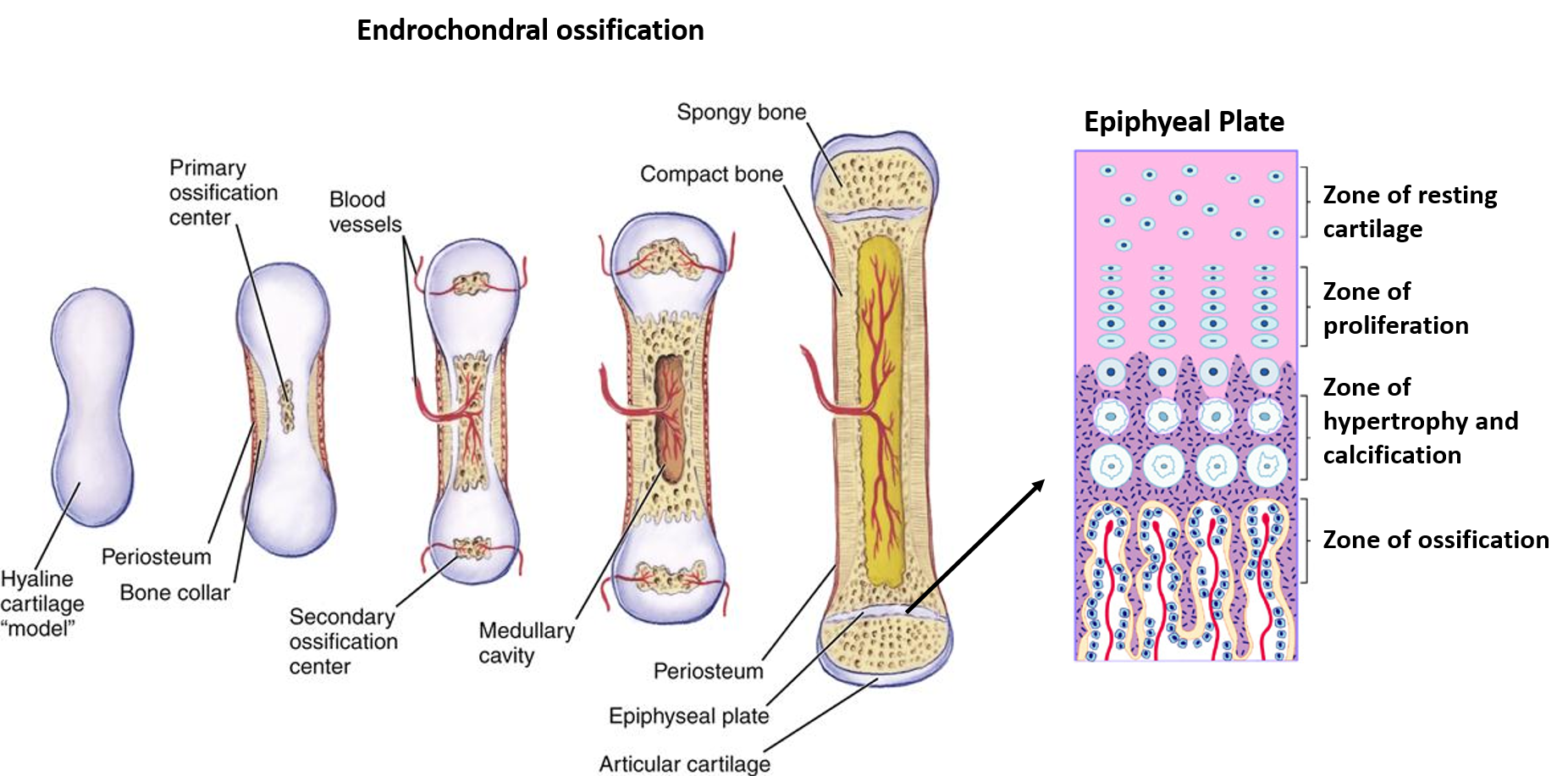
Formation of bone in subperiosteal area of diaphysis continues to increase thickness of the bone (appositional growth). The growth of bone in length occurs at (interstitial growth).
Five steps can summarize endochondral ossification:
- Mesenchymal cells differentiate into chondrocytes and form the cartilage model for bone.
- Chondrocytes near the center of the cartilage model undergo hypertrophy and alter the contents of the matrix they secrete, enabling mineralization.
- Chondrocytes undergo apoptosis due to decreased nutrient availability, blood vessels invade and bring osteogenic cells
- Primary ossification center forms in the diaphyseal region of the periosteum called the periosteal collar
- Secondary ossification centers develop in the epiphyseal region after birth.
What are the laws of ossification?
Following are Laws of ossification:
1. Primary center of ossification appears before birth and is usually single.
Exception –
- Carpals and tarsals ( cuneiforms, navicular) ossifiy after birth.
- Clavicle has 2 primary centers of ossification.
2. Secondary centres of ossification appear after birth and can be can be single or multiple.
Exception –
- Lower end of femur and upper end of tibia (secondary centers at these ends appear before birth, at the end of the 9th month of intrauterine life).
3 The direction of the nutrient foramen is opposite to the direction of the growing end of the bone.
4. The secondary center of ossification for pressure epiphysis appear before that of traction epiphysis (center of ossification in head of humerus (pressure epiphysis) appears before that in greater /lesser tubercles (traction epiphyses)).
5. The secondary center of ossification that appears first, fuses last with the shaft of long bone.
Exception –
- Lower end of fibula (secondary center for the upper end appears later but the secondary center for the lower end which appears first fuses earlier with the shaft of fibula).
6. The secondary centers fuse together to form a single epiphysis (compound epiphysis), which in turn fuses with the diaphysis.
Exception – Upper end of femur has 3 secondary centers, one each for the head , greater trochanter and lesser trochanter. Each epiphysis fuses independently (examples of simple epiphysis) with the shaft in the reverse order of appearance i.e the lesser trochanter at about 13 years first, followed by the greater trochanter at about 14 years, and the head around 16 years.
Applied Aspect
Anatomical basis of Cleidocranial dysostosis
A defect in membranous ossification causes Cleidocranial dysostosis in which ossification of bones ossifying in membrane that is clavicle and bones of skull vault are affected. It is characterised by aplasia of clavicle, increase in transverse diameter of cranium and retardation of ossification of fontanelle.
Anatomical basis of Dwarfism/Achondroplasia
A defect in endrochondral ossification affects growth and ossification of bones of limbs, which is responsible for dwarfism/achondroplasia in which the limbs are short but the trunk is normal. It may be inherited as autosomal dominant genetic disorder.
Why metaphysis is the common site of osteomyelitis in children?
Metaphysic is the area of very active growth of the bone and has rich blood supply. Before fusion of epiphysis with diaphysis i.e. in children, the metaphyseal arteries are end arteries that form ‘hair-pin bends’. The bacteria or infected emboli can be easily trapped in these hair- pin bends of the metaphyseal arteries causing osteomyelitis.


You come up with some great points within this article, but aren’t you forgetting something crucial?
Can I print these note
They are really great
woah. Thank you!