Where is Thyroid Gland Located?
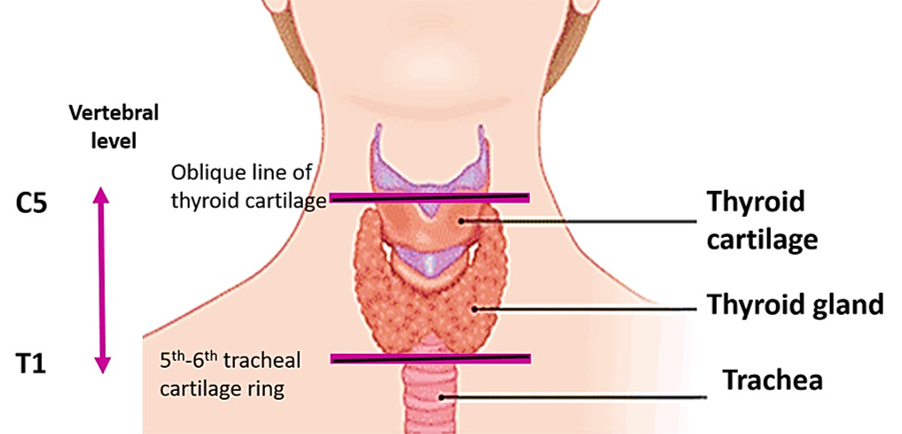
Thyroid gland, the largest endocrine gland is located in the lower part of neck anterolateral to the trachea. It extends from the oblique line of thyroid cartilage to the 5th-6th tracheal cartilage ring ( Lies opposite to the C5, C6, C7 and T1 vertebrae).
What are the parts of Thyroid Gland?
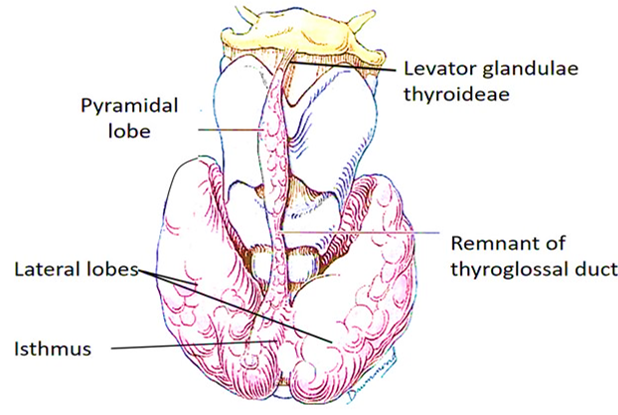
- Thyroid gland is H-shaped and consists of two lateral lobes connected by isthmus.
- A small pyramidal lobe may extend upwards from the upper border of the isthmus, slightly to the left of the midline.
- Sometimes the pyramidal lobe is connected to the hyoid bone by a fibromuscular band called levator glandulae thyroideae (remnant of thyroglossal duct).
- Each lobe extend above up to the oblique line of thyroid cartilage and below till the 5th or 6th tracheal cartilage ring.
- Isthmus lies in front of the 2nd-4th tracheal rings.
Dimensions of thyroid gland: Thyroid gland weighs approximately 25 gms. Each lobe of thyroid gland is 5 cm long, 3 cm wide and 3cm thick.
Describe the capsules of Thyroid Gland.
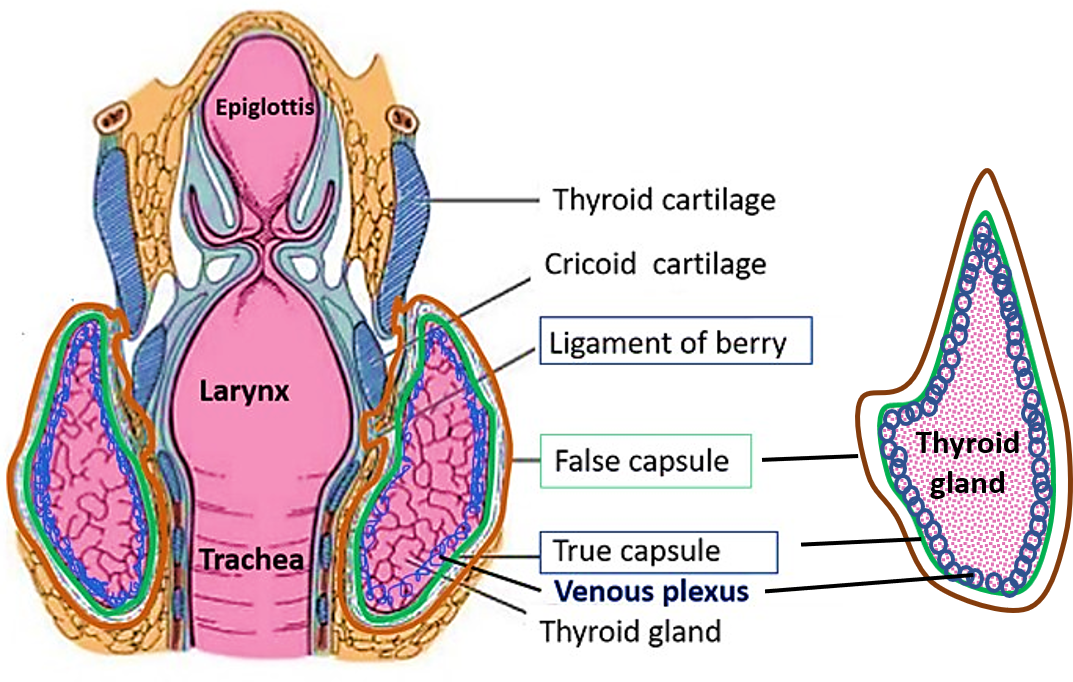
Thyroid gland is enclosed in two capsules:
- An inner true capsule which is formed by condensation of fibrous stroma of the gland.
- An outer false capsule which is formed by the pretracheal layer of the deep cervical fascia. It is thin along the posterior border of the lobes and thick on the medial surface of the lobes. The pretracheal fascia is attached above to the body of the hyoid bone and oblique line of the thyroid cartilage and after enclosing the thyroid gland it descends down in front of the trachea and blends with fibrous pericardium. On the medial surface of thyroid lobe it thickens to form the suspensory ligament of Berry, which attaches the lobe to the cricoid cartilage.
Describe the gross features and relations of Thyroid Gland.
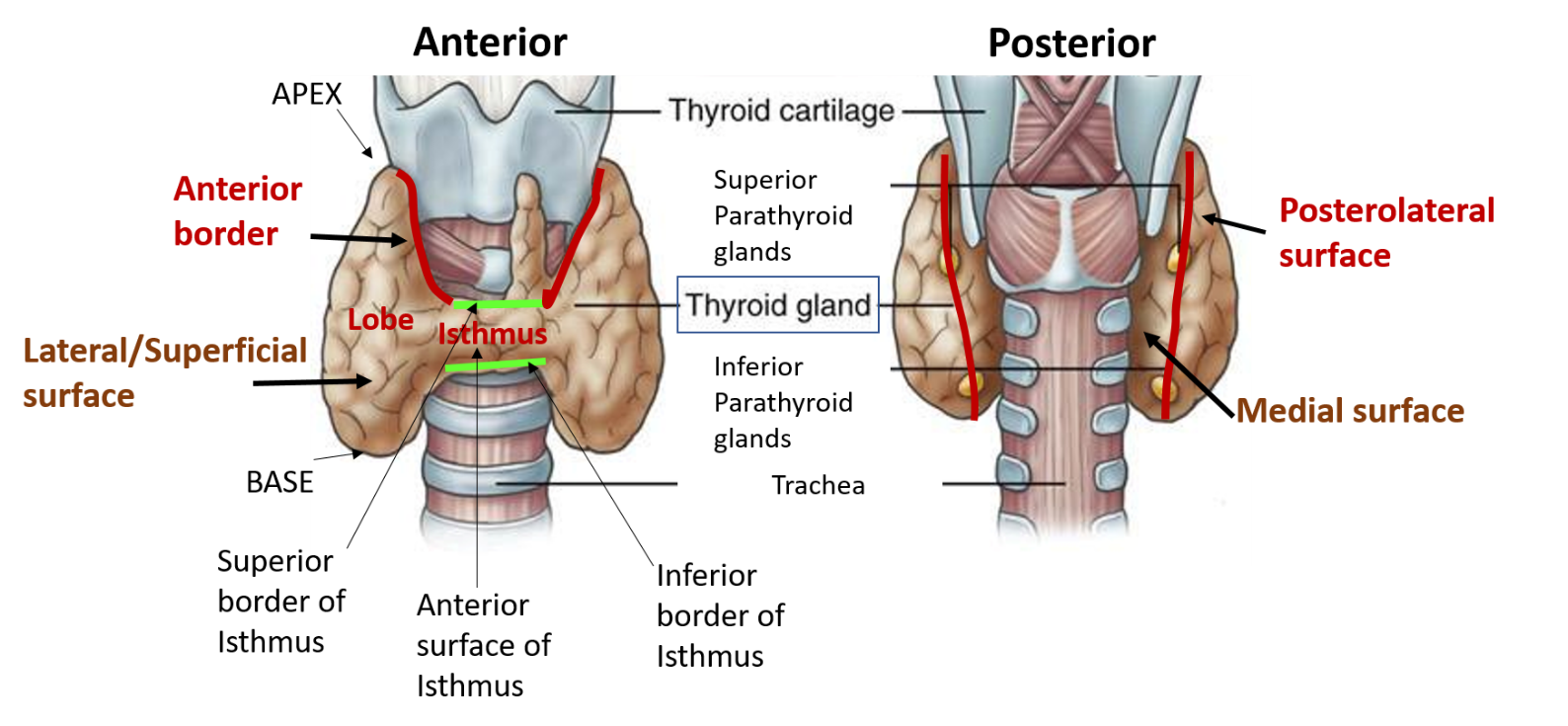
Thyroid gland presents two lateral lobes ( right and left) and median isthmus connecting the two lobes. Each lobe of thyroid gland is pyramidal in shape and has:
- Apex/Upper pole: it is directed upwards and laterally and extends till oblique line of thyroid cartilage. Lies opposite to C5 vertebra.
- Base/Lower pole: it extends upto the 5th or 6th tracheal cartilage ring. Lies opposite to T1 vertebra.
- Three Surfaces: lateral (superficial), medial and posterolateral
- Two Borders: anterior and posterior
Isthmus of thyroid gland has:
- Two surfaces: anterior and posterior
- Two borders: superior and inferior
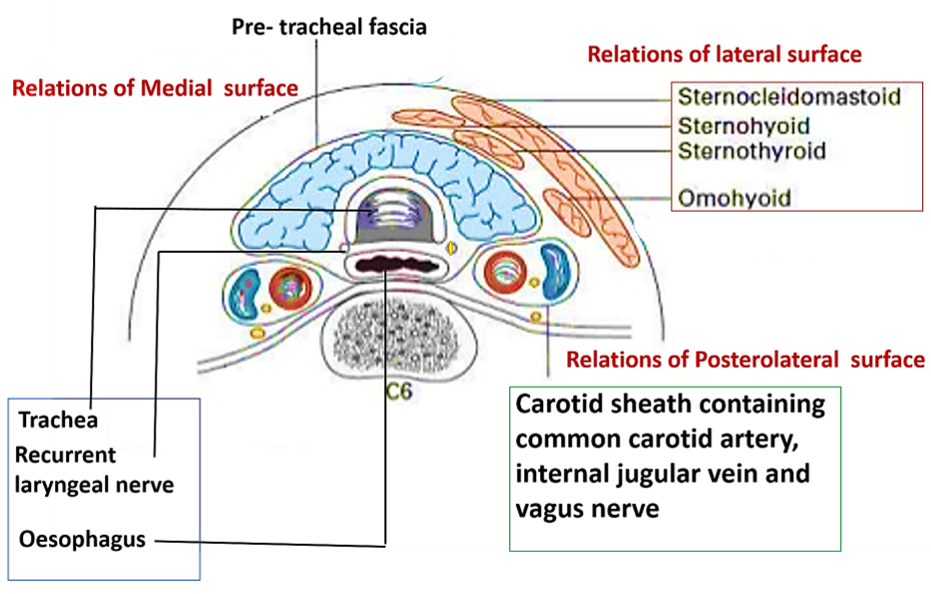
Relations of Thyroid Gland
Each lobe of thyroid gland has following relations:
- Apex/Upper lobe: is sandwiched between the sternothyroid and inferior constrictor muscle of pharynx. Superior thyroid artery and external laryngeal nerve diverge from each other close to upper pole. The artery is superficial and nerve lies deep to the upper pole.
- Base/Lower pole: is related to inferior thyroid artery and recurrent laryngeal nerve.
- Lateral (superficial) surface is related to the following muscles:
- Sternohyoid, sternothyroid, superior belly of omohyoid and anterior border of sternocleidomastoid.
- Medial surface is related to:
- Two tubes– trachea and oesophagus
- Two muscles – inferior constrictor and cricothyroid
- Two cartilages – cricoid and thyroid
- Two nerves – external laryngeal and recurrent laryngeal
- Posterolateral surface is related to:
- Carotid sheath and its contents (common carotid artery, internal jugular vein and vagus nerve). Ansa cervicalis is embedded in the anterior aspect of carotid sheath.
- Anterior border is thin and is related to anterior branch of superior thyroid artery.
- Posterior border is thick and rounded and is related to parathyroid glands and anastomosis between superior and inferior thyroid arteries.
Isthmus of thyroid gland has following relations:
- Anterior surface is related to sternothyroid and sternohyoid muscles and anterior jugular veins.
- Posterior surface is related to 2nd -4th tracheal rings.
- Superior border is related to anastomosis between anterior branches of superior thyroid arteries.
- Inferior border is related to inferior thyroid veins that leave isthmus along this border.
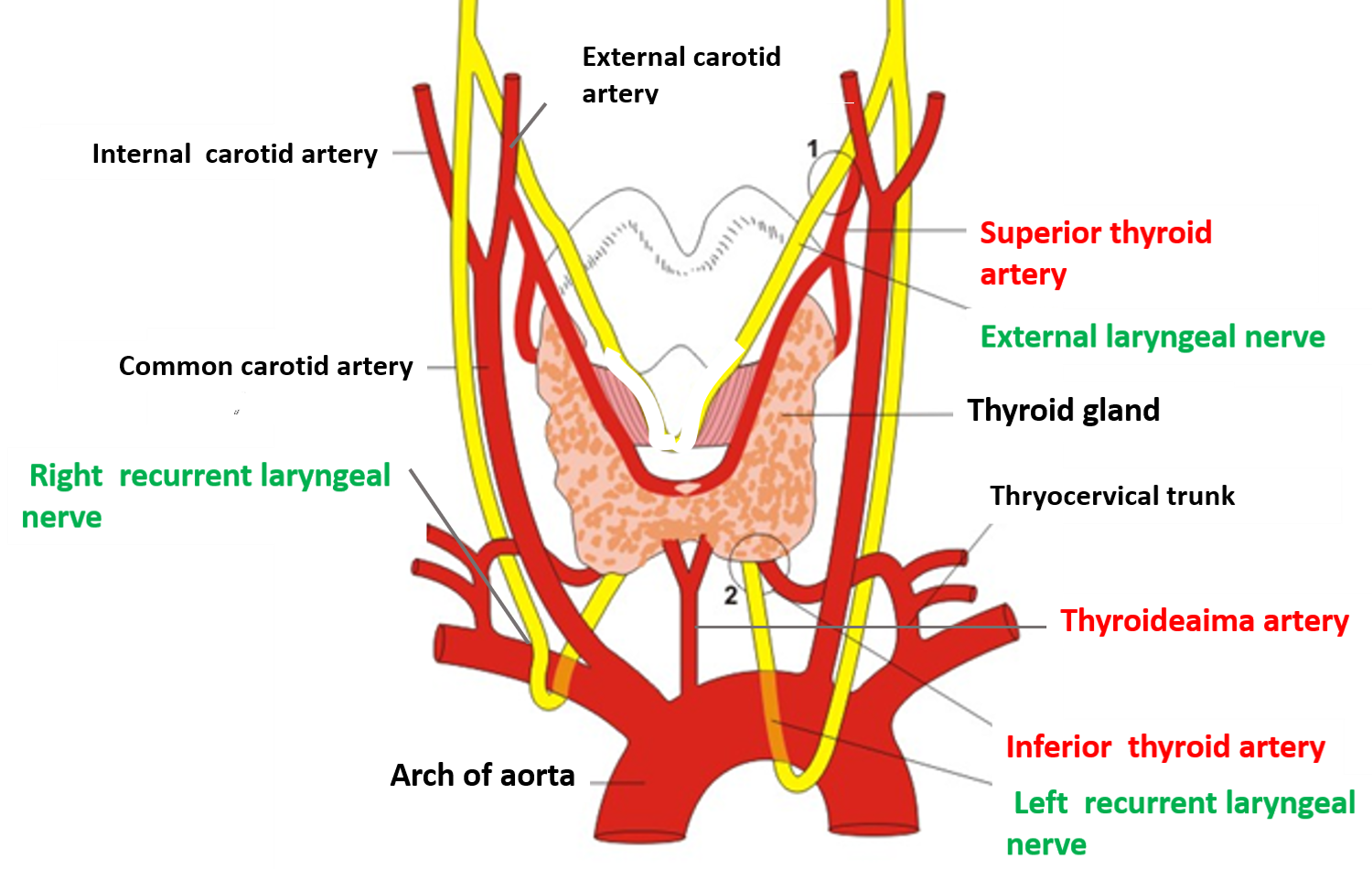
Describe briefly the arterial supply of Thyroid Gland.
Thyroid gland is highly vascular and is supplied by the following arteries.
- Superior thyroid artery:
- It is a branch of external carotid artery.
- Descends down to the upper pole of lateral lobe of thyroid gland accompanied by external laryngeal nerve (the nerve diverges from the artery near the upper pole).
- At the apex of lateral lobe, it divides into anterior and posterior branches.
- Anterior branch descends along anterior border and anastomoses with the its fellow of opposite side along the superior border of isthmus.
- Posterior branch descends along posterior border and anastomoses with the ascending branch of inferior thyroid artery.
- It supplies upper 2/3rd of the lobe and upper ½ of the isthmus.
- Inferior thyroid artery:
- It is a branch of thyrocervical trunk.
- It first runs upwards, then passes behind the carotid sheath and descends to reach the base of thyroid gland (forms a loop with convexity upwards).
- Near the base (lower pole) the artery is very close to recurrent laryngeal nerve.
- It supplies the lower 1/3rd of the lobe and lower half of the isthmus.
- Thyroideaima artery:
- It is a branch of brachiocephalic trunk or arch of aorta.
- Ascends in front of trachea to enter the isthmus.
- It is not always present.
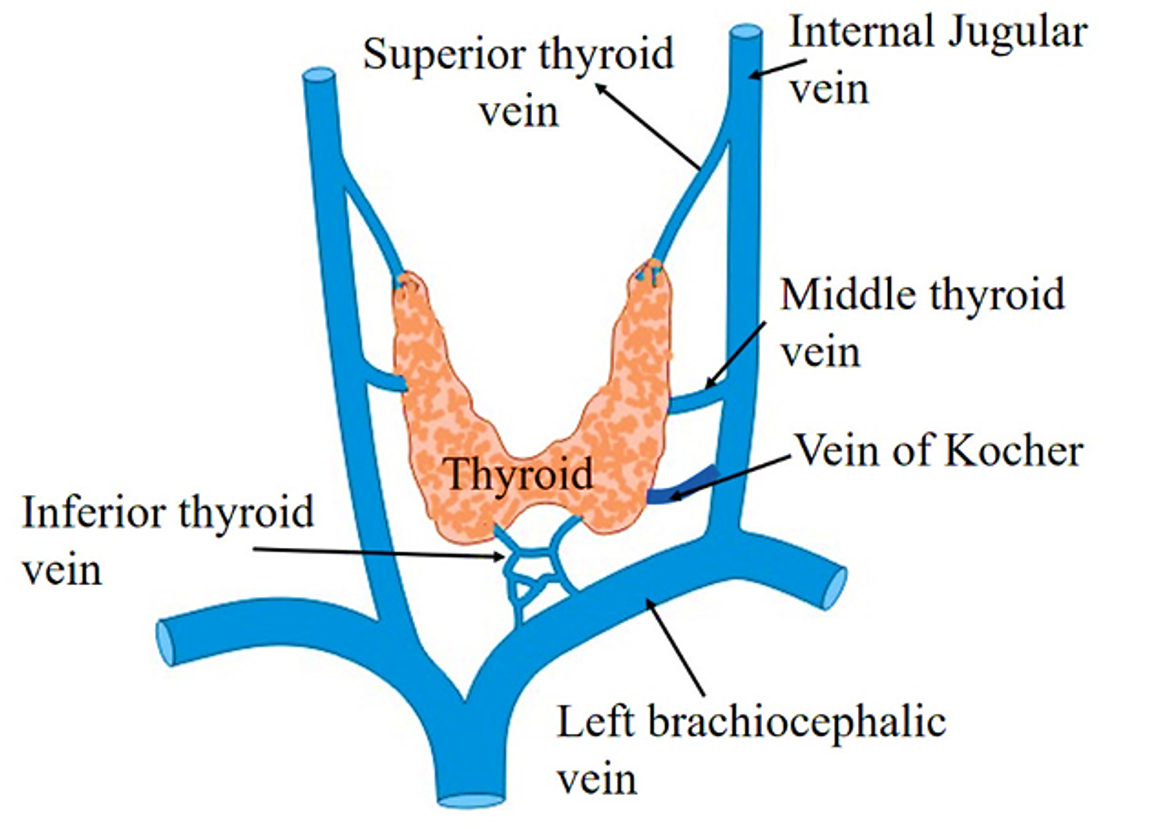
Name the veins that drain Thyroid Gland.
Venous drainage of thyroid occurs mainly via 3 pairs of veins. All thyroid veins do not accompany arteries. The three pairs of veins arise from the venous plexus present deep to the true capsule of thyroid gland.
- Superior thyroid veins emerge at the upper pole of thyroid gland and terminates in internal jugular vein.
- Middle thyroid veins are short veins, emerges at the middle of the lobe of thyroid gland and drains in internal jugular vein.
- Inferior thyroid veins emerge at the lower border of isthmus, descend in front of trachea (right and left vein communicate and form plexus in front of trachea) to drain into left brachiocephalic vein.
- Vein of Kocher: Sometimes a fourth vein (Vein of Kocher) emerges between the middle and inferior thyroid veins which drains into internal jugular vein.
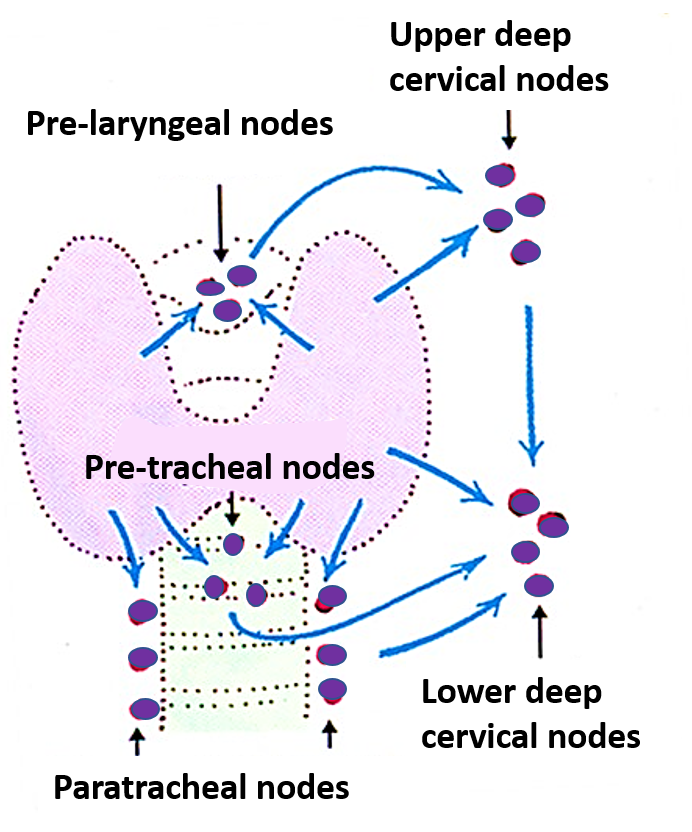
Describe briefly the lymphatic drainage of Thyroid Gland.
Lymphatics from the upper part of thyroid gland drain into pre-laryngeal and upper deep cervical lymph nodes. From the lower part of thyroid gland, the lymphatics drain into pretracheal, paratracheal and lower deep cervical lymph nodes.
Applied Aspect
Thyroid swellings move up and down during deglutition/swallowing.
The pretracheal fascia after enclosing the thyroid gland is connected to the oblique lines of the thyroid cartilage and the body of the hyoid bone. On the medial surface of thyroid lobe it thickens to form the suspensory ligament of Berry, which attaches the lobe of thyroid gland to the cricoid cartilage. As a result when larynx moves up and down during deglutition (the larynx is raised, along with the pharynx, by the contraction of the longitudinal muscles of the pharynx that are attached on the posterior border of thyroid cartilage), thyroid gland also moves. This help in distinguishing the thyroid swelling from other swellings in the neck.
Thyroid gland is removed along with its true capsule.
In case of thyroid gland , the venous plexus is located deep to the true capsule. Therefore, to avoid hemorrhage during thyroidectomy, the thyroid gland is removed together with the true capsule. Whereas, in case of prostate gland, the venous plexus is located between its true and the false capsules and therefore, during surgical removal of prostate gland (prostatectomy) prostate gland is removed leaving behind both the capsules.
Superior thyroid artery is ligated close to thyroid gland.
Superior thyroid artery lies close to the external laryngeal nerve in its proximal part and they diverge near the apex of lateral lobe (artery is superficial and the nerve is deep to the apex). Therefore, during thyroidectomy the superior thyroid artery should be ligated close to the apex to avoid injury to the external laryngeal nerve.
Inferior thyroid artery is ligated away from the thyroid gland.
Inferior thyroid artery is very close to the recurrent laryngeal nerve near the base/lower pole of the thyroid gland. Therefore, during thyroidectomy it should be ligated away from the inferior pole of thyroid gland to avoid injury to the recurrent laryngeal nerve.
Goitre
The enlargement of thyroid gland is termed ‘goitre’. Endemic goiter occurs due to deficiency of iodine in the diet (decreased levels of T3 and T4). Such goiters present symptoms and signs of hypothyroidism.Toxic goiters /thyrotoxicosis occurs due to excess secretion of T3 and T4 and clinically presents as – increased BMR , tremors, tachycardia. Enlarged thyroid tends to grow either backwards or downwards. Patients with large goitre present with classical symptoms of
- Dysphonia (hoarseness of voice)
- Dysnoea (difficulty in breathing)
- Dysphagia (difficulty in swallowing)
Cretinism and Myxedema
Hypofunction of thyroid in infants and children is called cretinism and in adults, is called myxedema.
Partial Thyroidectomy
In partial thyroidectomy the posterior part of thyroid lobes are left behind to avoid removal of parathyroid glands which otherwise may result in tetany.
very good site
well-organized!