EXTRA-EMBRYONIC MEMBRANES AND PLACENTA
Q. What are the structures marked 1- 10 in the following diagram.

Q. What is amniotic fluid and how it is produced?
A. Amniotic fluid is clear and watery fluid present in the amniotic cavity. It is produced by:
- maternal plasma which diffuses across fetal membranes.
- some amount is secreted by amnioblasts lining the amniotic cavity.
- when fetal kidney becomes functional, fetal urine also contributes to it.
Q. What is the normal amount of amniotic fluid at 36 weeks?
A. By 36 weeks about 1000 ml amniotic fluid is present.
Q What is Oligohydroamnios?
A. It is a condition when the amniotic fluid is less than 400 ml at 36 weeks. One of the commonest cause is renal agenesis.
Q. What is polyhydroamnios?
A. It is a condition when there is more than 2000 ml of amniotic fluid at term pregnancy. It occurs usually due to esophageal atresia or anencephaly in which fetus is unable to swallow the amniotic fluid.
Q. What are the functions of amniotic fluid?
A. Following are the functions of amniotic fluid.
- Provides watery cushion to absorb shock and protect the embryo/fetus against mechanical injury.
- Allows symmetrical development/growth of fetus.
- Allows fetus to move freely. Prevent adherence of fetus to amnion.
- Maintains constant temperature.
- Provides hydrostatic mechanism in the widening of the cervix in the early stages of labor.
- Protective cushion against the pressure from uterine contraction during labor.
Q. What is allantois and what is its fate?
A. It is a diverticulum from the caudal end of the yolk sac that projects into the connecting stalk.
Its Significance:
- Blood cell formation occurs in its walls during 3-5th week of development.
- It is vasularized by allantoic vessels which later become umbilical arteries and vein.
Its fate : Its intraembryonic part connects the umbilicus to the apex of urinary bladder. It involutes to form urachus and after birth, the urachus becomes a fibrous cord called the median umbilical ligament.
Anomalies: It may persist as urachal cyst, sinus or fistula.
Q. What are the functions of yolk sac?
A. Following are the functions of yolk sac:
- Provides nutrition to the embryo during 2nd and 3rd weeks.
- Blood cell formation occurs in its walls from 3rd week onwards till 5th week when the haemopoietic activity begins in liver.
- During 4th week its dorsal part is incorporated into the embryo as primitive gut and that gives rise to the epithelium of trachea, bronchi, lungs, digestive tract, parenchyma of thyroid, parathyroid, liver and pancreas, epithelial lining of tympanic cavity and auditory tube.
- Primordial germ cells appear in the yolk sac wall in the 3rd week and migrate to the area of developing gonads ( abdomen) where they become oogonia and spermatogonia.
Q. What are the contents of umbilical cord?
A. Following are the contents of umbilical cord:
- Two umbilical arteries
- One umbilical vein
- Vitello-intestinal duct and remnants of yolk sac
- Wharton’s jelly – extraembryonic mesoderm of the connecting stalk that is rich in hyaluronic acid.
Q. What are the dimensions of umbilical cord at full term?
A. Length is about 50 -60 cm and the diameter is about 2cm.
Q. What is the fate of umbilical arteries and vein in adults?
A. Umbilical arteries proximal part forms vesical arteries supplying urinary bladder and distal part form medial umbilical ligaments. Left umbilical vein forms ligamentum teres hepatis.
Q. What are the components of placenta?
A. Placenta is an organ of dual origin and consists of fetal and maternal components.
- Fetal part is formed by chorion frondosum ( part of chorion in which chorionic villi persist).
- Maternal part is formed by decidua basalis ( part of endometrium of uterus).
Q. What is decidual reaction and decidua? A. After implantation the syncytiotrophoblast starts secreting HCG ( Human Chorionic Gonadotropin) . Under the influence of HCG the secretory phase in endometrium is intensified and the endometrial cells around the conceptus enlarge and acquire lipid and glycogen. this change in the endometrium stroma is called decidual reaction. . The endometrial cells are called decidual cells and the endometrium is now called decidua.
Q. What are the parts of decidua?
A. Following are the parts of Decidua:
- Decidua basalis: That part of endometrium which lies deep to the implanted blastocyst. It contributes to the maternal component of placenta.
- Decidua capsularis: Part of the endometrium that surrounds the embryo like a cap and separates it from the uterine cavity.
- Decidua Parietalis: Part of the endometrium that lines the rest of the uterine cavity.
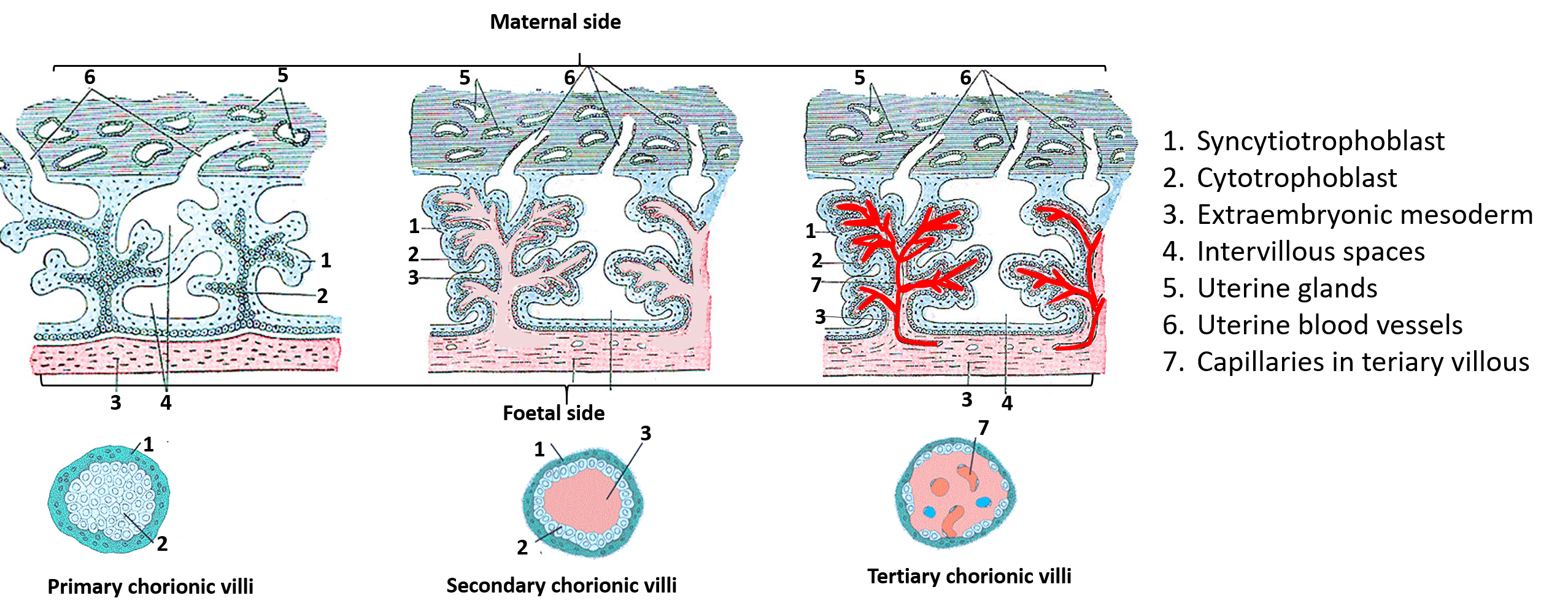
Q. What are the stages in the formation of chorionic villi?
A. Finger like processes on the outer surface of chorion are called chorionic villi. Chorionic villi in relation to the decidua basalis grow extensively and this part of the chorion is called chorion frundosum. It contribute to the formation of fetal part of placenta. There are three stages in the formation of chorionic villi:
- Primary chorionic villi: They consist of a central core of cytotrophoblast covered by a layer of syncytiotrophoblast. These villi are separated from each other by the intervillous spaces filled with maternal blood.
- Secondary chorionic villi: These are formed in the early 3rd week. They are formed as extraembryonic mesoderm (EEM) grows and penetrate the core of primary chorionic villi. As a result the secondary villi have three layers- Inner layer of extraembryonic mesoderm, intermediate layer of cytotrophoblast and outer layer of syncytiotrophoblast.
- Tertiary chorionic villi: They are formed at the end of the 3rd week. They are formed due to the differentiation of mesenchymal cells of EEM into blood capillaries and blood cells. Thus they have all the layers of secondary villi along with the blood vessels in the extraembryonic mesoderm.
Q. Name the structures marked 1- 7 in the following diagram.
Q. What are the features of full term placenta?
A. Gross features of full term placenta are as follows:
- Shape is discoid.
- Diameter is ` 20cm.
- Thickness is ` 2.5 cm.
- Weight is ` 500 gm.
- Surfaces – There are two surfaces, material and fetal. Maternal surface is divided into 15-20 cotyledons by decidual septa. Fetal surface is smooth and covered with amnion. Umbilical cord is attached eccentrically to this surface. Umbilical vessels ramify under the amnion.
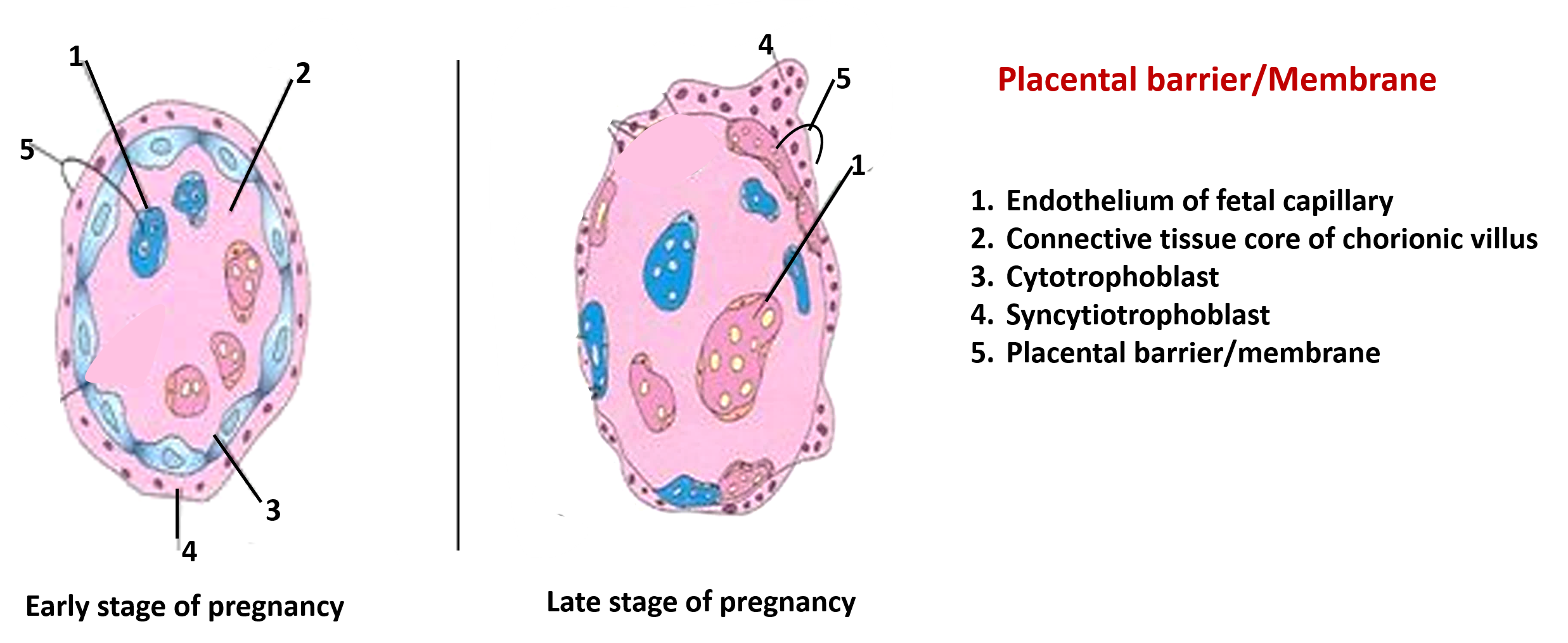
Q. Name the structures that form placental barrier.
A. In the early part of the pregnancy the placental barrier or membrane is made of the following layers. From the fetal side they are:
- Endothelium of fetal blood vessels and its basement membrane
- Surrounding connective tissue ( extraembryonic mesoderm)
- Cytotrophoblast and its basement membrane
- Syncytiotrophoblast
In the later part of the pregnancy the thickness is reduced due to:
- Disappearance of cytotrophoblast
- Peripheral migration of fetal blood vessels
- thinning of syncytiotrophoblast
As a result the placental membrane comprises of :
- Fetal endothelium with its basement membrane
- Syncytiotrophoblast
Q. Name the structures labeled 1- 5 in the following diagram.
Q. What are the functions of placenta?
A. It has following functions:
- Allows transport of oxygen, water, electrolyte and nutrients ( carbohydrates, lipids, amino acids, vitamins etc.) from maternal blood to fetal blood.
- Eliminates/excretion of carbon dioxide, urea and other waste products produced by the fetus into maternal blood.
- Acts as a barrier and to many pathogens- bacteria and other harmful substances (however most viruses – such as poliomyelitis, rubella, measles and some bacteria can pass across it.
- Maternal antibodies (IgG) reach the fetus through placenta that provide the fetus immunity against some infections such as diphtheria and measles.
- Hormones produces by placenta ( syncytiotrophoblast) such as 1) progesterone is essential for the maintenance of pregnancy after the 4th month and 2) estrogen which reaches maternal blood promotes uterine growth and development of mammary gland.
Q. Which harmful substances may cross the placental barrier and reach fetus?
A. The following may cross the placental barrier:
- most viruses – such as poliomyelitis, rubella, measles and some bacteria can pass across it.
- Maternal hormones do not reach the fetus, however, synthetic progestins and estrogens can easily cross the placental barrier and have adversely affect fetus.
- Certain drugs cross the placental barrier and can cause congenital malformation e.g. Thalidomide.
Q. What is placenta previa?
A. Normally the implantation occurs in the upper uterine segment. if the implantation occurs in the lower part of the uterine cavity, the placenta partially or completely covers the internal Os of cervix. This condition is called placenta previa. It is common cause of bleeding in later part of gestation and during parturition. There are four degrees of placenta previa:
- First degree: Placenta is attached to the lower uterine segment but does not cover the internal Os.
- Second degree: Attachment of placenta reaches the margin of internal Os.
- Third degree: Placenta partially covers the internal Os but when cervix dilates at the time of birth , it does not occlude the internal Os.
- Fourth degree: Placenta completely covers the internal Os.
Excellent presentation
This is very helpful thank you very much